einstein (São Paulo). 14/Mar/2025;23(spe1):eAO1060.
Assessment of mortality due to severe SARS-CoV-2 infection in public and private intensive care units in Brazil: a multicenter retrospective cohort study
DOI: 10.31744/einstein_journal/2025AO1060
Highlights
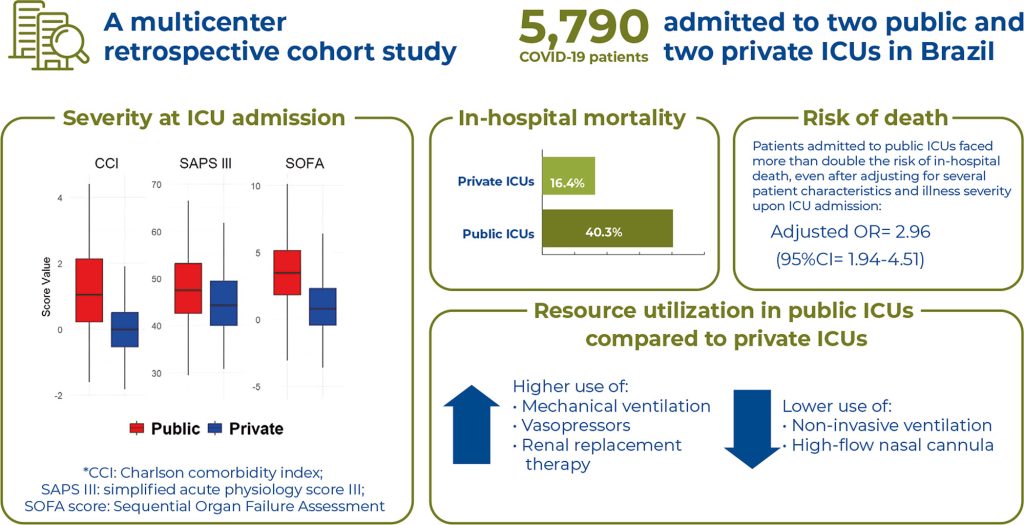
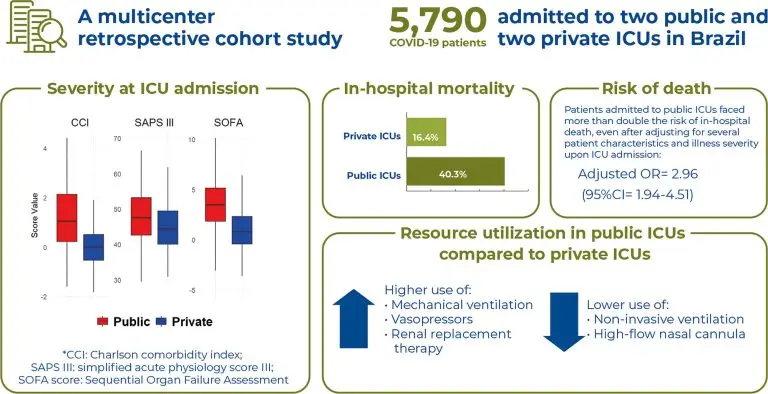
■ Public intensive care unit COVID-19 patients presented with more comorbidities and higher severity at admission.
■ Public intensive care units required more invasive organ support (e.g., mechanical ventilation, vasopressors, and renal replacement therapy) but less non-invasive ventilation and high-flow nasal cannula than private intensive care units.
■ In-hospital mortality was higher in public intensive care units, with an increased risk of death even after adjusting for patient characteristics and illness severity at intensive care unit admission.
ABSTRACT
Objective:
To compare the clinical characteristics, use of organ support, and outcomes of critically ill patients with COVID-19 admitted to public and private intensive care units.
Methods:
This multicenter retrospective cohort study included patients admitted to four intensive care units from March 1, 2020, to December 31, 2021. Patients with COVID-19 admitted to public and private intensive care units were compared. The primary outcome of interest, in-hospital mortality, was assessed using a hierarchical logistic regression (multilevel) model adjusted for study site and patient characteristics.
Results:
A total of 5,790 patients with COVID-19 were admitted to the participating intensive care units, with 3,321 (57.3%) admitted to private hospitals and 2,469 (42.6%) admitted to public hospitals. Patients in public intensive care units were less likely to be male and had higher median SAPS III scores, Charlson Comorbidity Index values, and SOFA scores. They also required mechanical ventilation (53.1% versus 40.0%, p<0.001), vasopressors (43.1% versus 33.9%, p<0.001), and renal replacement therapy (20.3% versus. 14.5%, p<0.001) more frequently than those in private intensive care units. In contrast, patients in private intensive care units were more frequently managed with non-invasive ventilation (38.0% versus 66.8%; p<0.001) and high-flow nasal cannulas (18.3% versus 48.1%; p<0.001). The in-hospital mortality rate was significantly higher in public intensive care units (40.3%) compared to private intensive care units (16.4%) (adjusted OR=2.96; 95%CI=1.94-4.51; p<0.001).
Conclusion:
We observed significant differences in resource utilization and mortality rates between patients with COVID-19 admitted to public and private intensive care units. Patients with COVID-19 in public care units face a higher risk of in-hospital mortality compared to those in private care units.
[…]
144