einstein (São Paulo). 28/Apr/2025;23:eAO1343.
Quality assessment of clinical practice in neuro-oncology
DOI: 10.31744/einstein_journal/2025AO1343
Highlights
■ The molecular test according to the WHO classification of CNS tumors (gliomas) was performed in 100% (172) of patients.
■ Education on chemotherapy and informed consent for patients with brain tumors was carried out for 100% (130) of the patients who had an indication for chemotherapy treatment.
■ Approximately 87% of the patients with gliomas underwent postoperative cranial MRI.
■ A multidisciplinary approach, including molecular testing, was used for 35% of patients with glioma.
■ Thromboembolic events after resection of the primary brain tumor occurred in only 0.84% (3) patients.
ABSTRACT
Objective:
To evaluate the quality indicators proposed by the American Academy of Neurology and Neuro-oncology Society in patients with primary intracranial central nervous system tumors.
Methods:
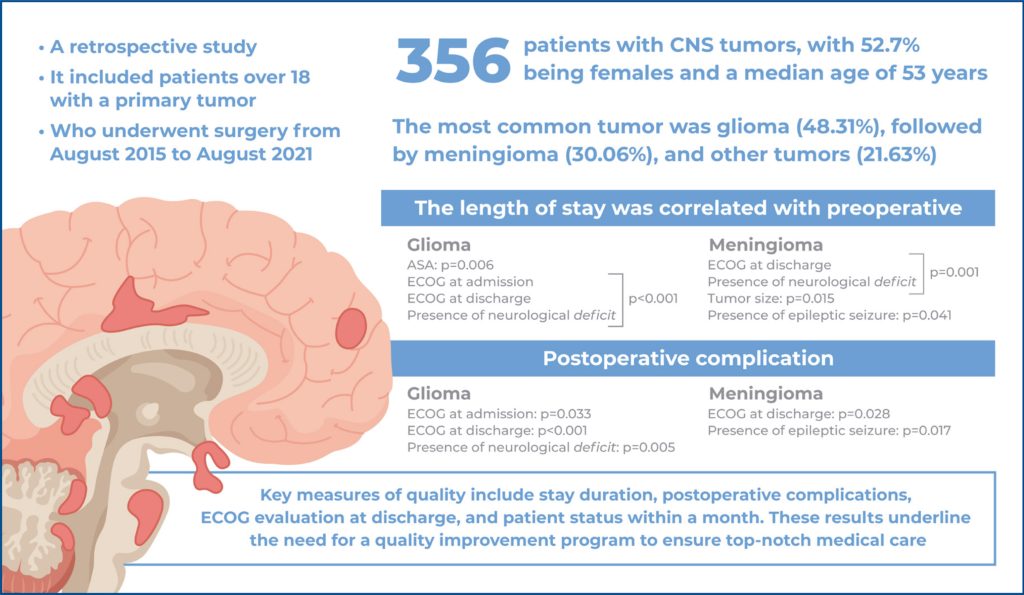
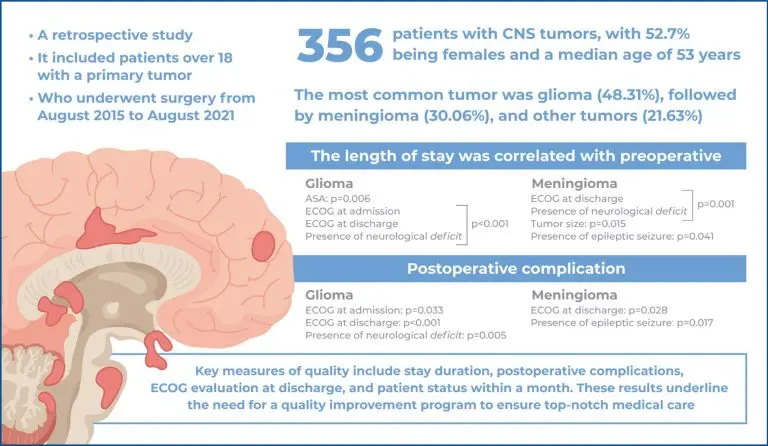
This study is a retrospective level I analysis that used electronic medical records from the CERNER system and GDOC-SAME at the tertiary hospital. It was approved by the Research Ethics Committee and followed the Declaration of Helsinki. Data was collected and analyzed confidentially via REDCap. The research focused on patients 18 or older with primary central nervous system tumors who had surgery from August 2015 to August 2021. It excluded surgeries performed elsewhere, reoperations, secondary (metastatic) tumors, and primary central nervous system tumors outside the cranium.
Results:
The results showed that 48% of the patients had gliomas, whereas 30 and 21.6% had meningiomas and other types of tumors. Quality measures showed that 35% of the patients with grade 2-4 tumors had multidisciplinary care plan discussions. All patients with gliomas underwent molecular testing and those eligible who underwent chemotherapy were educated and provided informed consent. Postoperative magnetic resonance imaging within 72h was performed in 87% of gliomas. The length of hospital stay, postoperative complications, Eastern Cooperative Oncology Group status at discharge, and 30-day status were also potential quality measures. However, for meningioma cases, readmissions were associated with patients in the American Society of Anesthesiologists II (58.33%) and American Society of Anesthesiologists III-IV (41.67%).
Conclusion:
The study conclusions revealed that adherence to quality indicators was good; however, improvements are needed in multidisciplinary care plans and postoperative imaging. Quality measures can be enhanced by controlling factors such as American Society of Anesthesiologists and Eastern Cooperative Oncology Group scales at admission, epileptic seizure occurrence, neurological deficits, and tumor size in meningiomas. The study’s findings highlighted the importance of quality improvement programs for optimal medical care.
[…]
146