einstein (São Paulo). 15/Dec/2021;19:eAI6683.
Scimitar syndrome: a rare disease
DOI: 10.31744/einstein_journal/2021AI6683
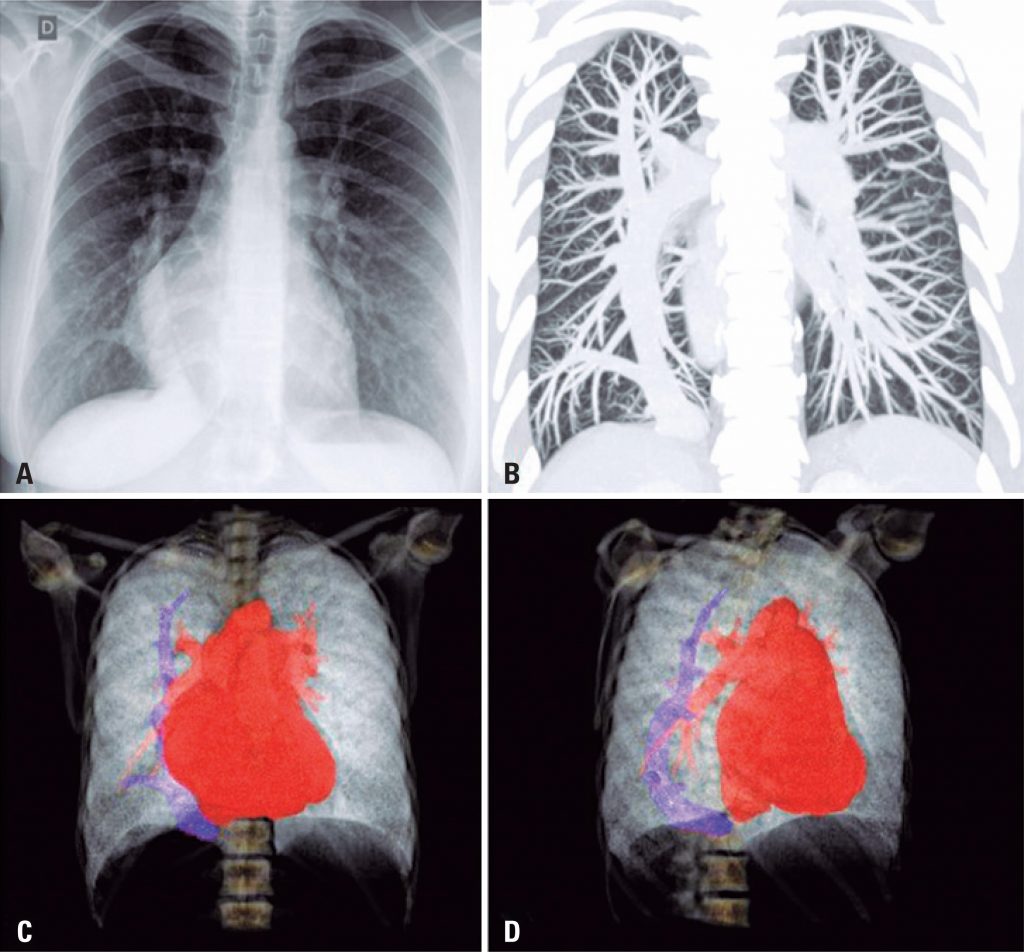
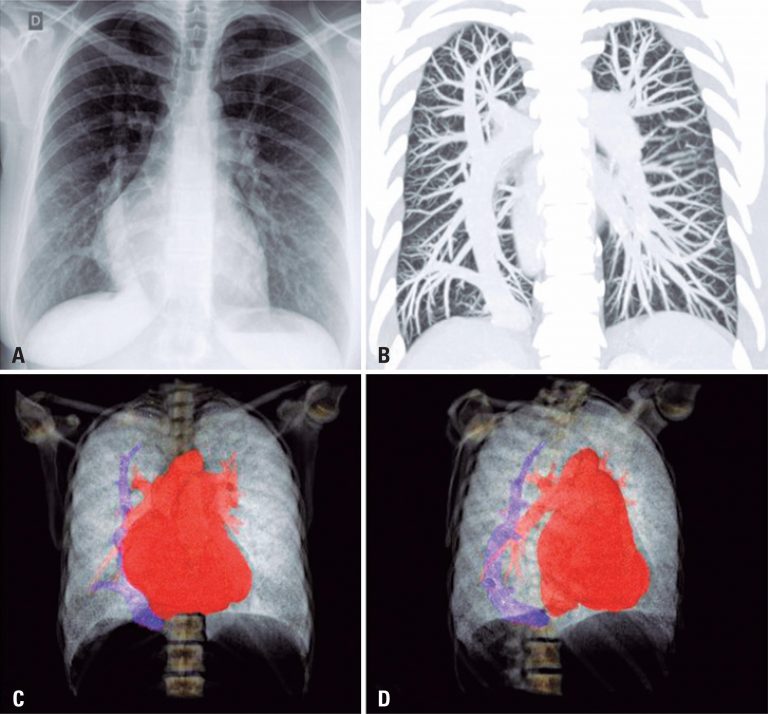
A 34-year-old patient with a history of asthma, taking inhaled corticosteroids and bronchodilators, presented with worsening dyspnea (functional class III) and reports of syncope. On physical examination, pulmonary auscultation was normal with pulse oximetry of 96% in room air. On cardiac auscultation, the rhythm was regular with fixed splitting S2 and systolic murmur 2+/6+ on left sternal border. On abdominal examination, the liver was palpable 2cm below the right costal border. There were no other signs of heart failure. Chest radiography was performed during the investigation, which showed a calibrous tubular structure slightly arched towards the right atrium and part of the cardiac area occupying the right hemithorax ( ). Chest CT scan revealed a large caliber anomalous vein in the right lung, draining into the cavoatrial junction ( ). Three-dimensional computed tomography scan using intravenous contrast showed a thick anomalous vein arched along the craniocaudal axis of the right lung, draining into the cavoatrial junction, compatible with scimitar ( and ).
The patient underwent right and left cardiac catheterization, which revealed an ostium secundum atrial septal defect (ASD) of 18mm, left-to-right flow with repercussions in the right chambers, and anomalous drainage of the right pulmonary veins into the inferior vena cava. A fine caliber arterial branch of the celiac trunk irrigated a small portion of the lower lobe of the right lung. Pulmonary hyperflow was shown with pulmonary artery pressure measurements of 30×15 and mean of 21, adequate pulmonary vascular resistance (PVR) of 0.95W, with pulmonary capillary wedge pressure of 10, and right atrial pressure of 8. Qp/Qs (pulmonary/systemic flow) was 1.74, indicating left-right shunt.
[…]
4,783