einstein (São Paulo). 30/Jul/2025;23:eGS0933.
Hospital costs of maternal near miss: a micro-costing analysis
DOI: 10.31744/einstein_journal/2025GS0933
Highlights
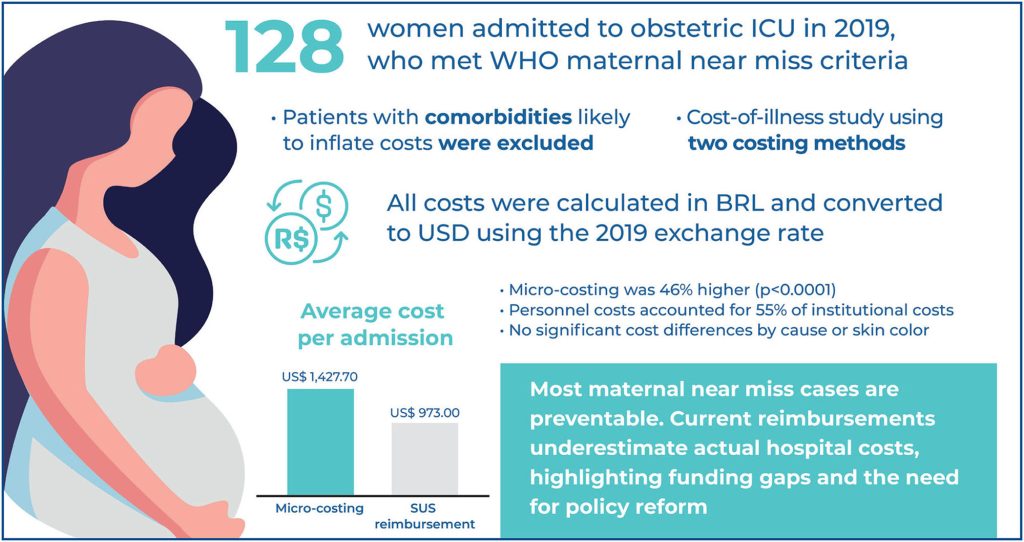
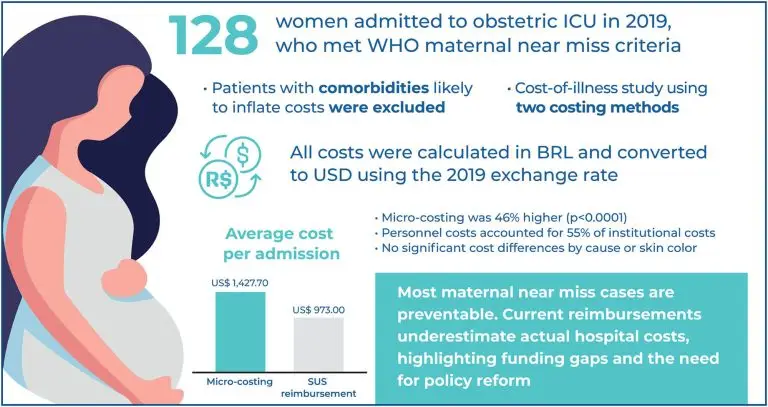
■ Micro-costing showed high per-admission costs (US$ 1,427.70) for maternal near miss.
■ Reimbursement values (US$ 973) underestimate true hospital costs.
■ Brazil’s economic burden estimated at US$ 86 million (2019).
■ Most maternal near miss events stem from preventable causes.
ABSTRACT
Objective:
This study aimed to estimate the hospital costs of maternal near miss cases from both the institutional and Brazilian Public Health System perspectives in a reference maternitiy hospital.
Methods:
This cost-of-illness study used primary data collected from 128 patients admitted to the obstetric intensive care unit of a reference hospital in 2019 who met the maternal near-miss criteria. Two costing methods were used: micro-costing assessment through reviewing medical records and micro-costing assessment derived from reimbursement data of the Brazilian Public Health System. The resources used were assigned costs in reais (R$) that were converted into US dollars (US$) based on 2019 values.
Results:
The average cost of a hospital stay for patients treated for maternal near miss was US$ 1,427.70 per medical record review and US$ 973.00 per Brazilian Public Health System reimbursement. The costs estimated by reimbursement were significantly lower than those estimated by reviewing medical records (p<0.0001). Considering the estimated incidence of maternal near miss among women treated in the Brazilian Public Health System, the projected national economic burden was US$ 86,055,130.50 in 2019.
Conclusion:
Through using a micro-costing methodology, this study established that, for the Brazilian Public Health System, hospital admissions due to maternal near misses had resulted in high costs, although this condition is considered to involve a large number of preventable cases. The cost estimates derived from the institution’s medical records were significantly higher than the estimated reimbursement costs.
[…]
72