28/Aug/2025
Elderly patients in crisis: unveiling outcomes and management approaches in severe COVID-19 cases – a retrospective analysis from Brazil
einstein (São Paulo). 28/Aug/2025;23:eAO1428.
View Article28/Aug/2025
Elderly patients in crisis: unveiling outcomes and management approaches in severe COVID-19 cases – a retrospective analysis from Brazil
DOI: 10.31744/einstein_journal/2025AO1428
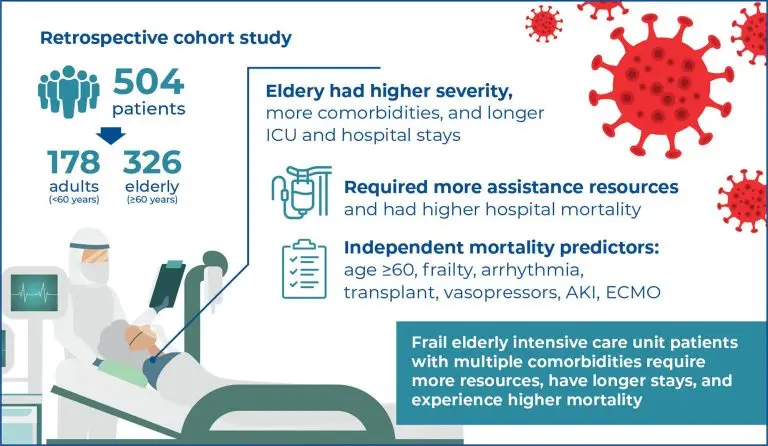
Highlights ■ The elderly had higher severity, more comorbidities, and longer intensive care unit and hospital stays than adults. ■ They required more assistance resources and had higher hospital mortality. ■ Independent mortality predictors: age ≥60, frailty, arrhythmia, transplant, acute kidney injury, vasopressors and extracorporeal membrane oxygenation. ABSTRACT Objective: To analyze the sociodemographic and clinical characteristics, comorbidities, therapeutic resources, and mortality rates of elderly patients with COVID-19 admitted to an intensive care unit. Methods: This retrospective cohort study included patients […]
Keywords: Acute kidney injury; Aged; COVID-19; Critical care outcomes; Hospital mortality; Intensive care units; Length of stay; Mortality
28/Aug/2023
Outcome prediction for critical care patients with respiratory neoplasms using a multilayer perceptron neural network
einstein (São Paulo). 28/Aug/2023;21:eAO0071.
View Article28/Aug/2023
Outcome prediction for critical care patients with respiratory neoplasms using a multilayer perceptron neural network
DOI: 10.31744/einstein_journal/2023AO0071
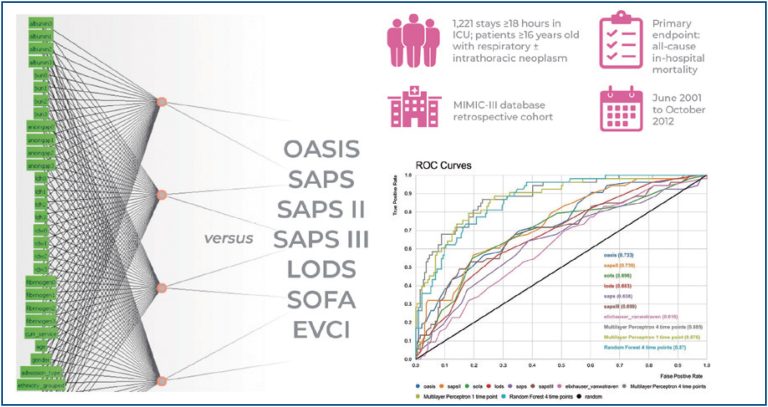
Highlights Two artificial neural networks, type of multilayer perceptron, and a random forest model were developed. Multilayer perceptron and random forest were compared to the OASIS, SAPS, SAPS II, SAPS III, LODS, SOFA, and EVCI Scores. Discrimination was assessed with the receiver operator characteristic and precision-recall curves. Calibration of the predictive models was evaluated with the Brier Score. ABSTRACT Objective The variation in mortality rates of intensive care unit oncological patients may imply that clinical characteristics and prognoses are very […]
Keywords: Artificial neural network; Hospital mortality; Intensive care units; Respiratory tract neoplasms; Survival
14/Jun/2022
Development and validation of predictive model for long-term hospitalization, readmission, and in-hospital death of patients over 60 years old
einstein (São Paulo). 14/Jun/2022;20:eAO8012.
View Article14/Jun/2022
Development and validation of predictive model for long-term hospitalization, readmission, and in-hospital death of patients over 60 years old
DOI: 10.31744/einstein_journal/2022AO8012
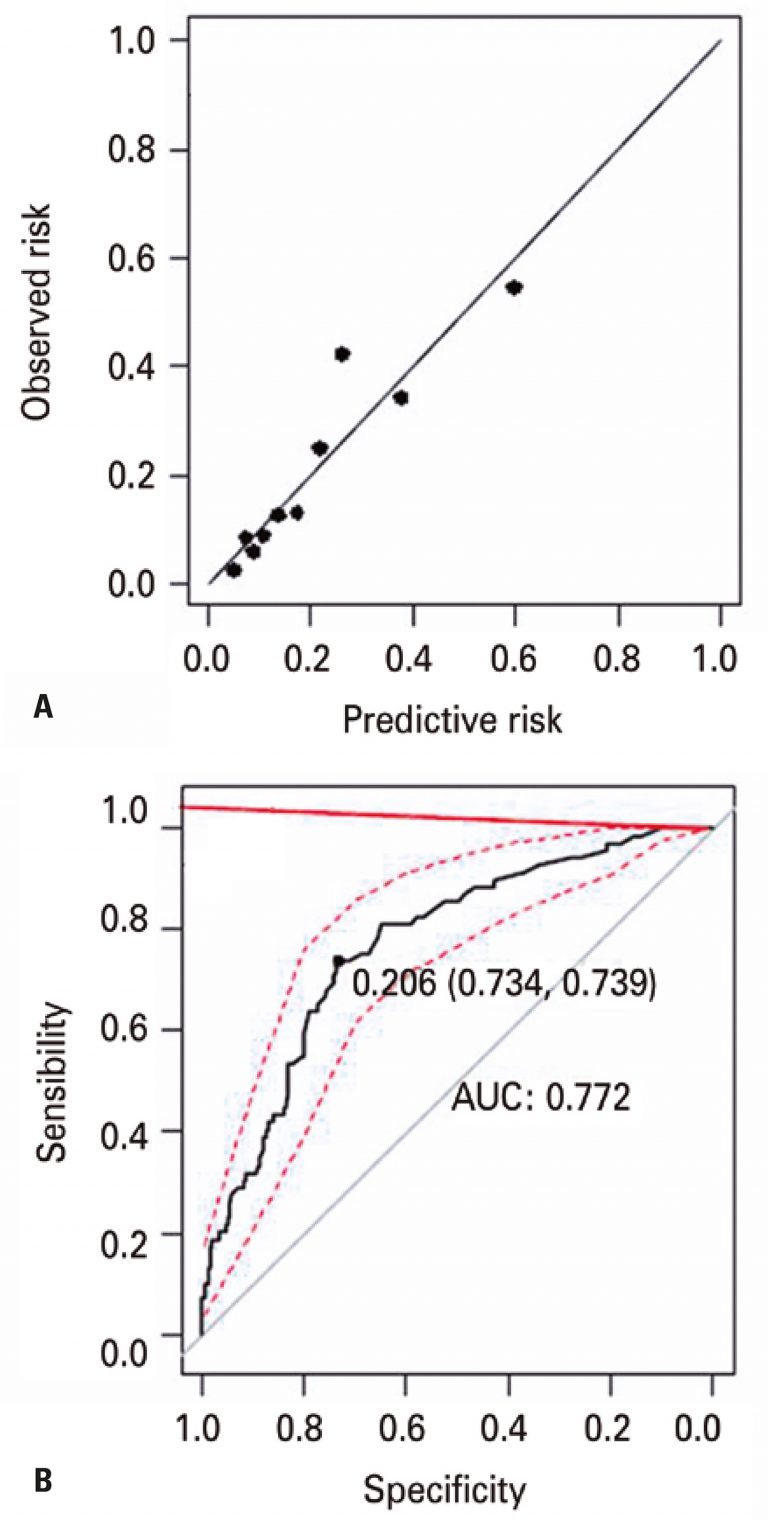
ABSTRACT Objective To develop and validate a high-risk predictive model that identifies, at least, one common adverse event in older population: early readmission (up to 30 days after discharge), long hospital stays (10 days or more) or in-hospital deaths. Methods This was a retrospective cohort study including patients aged 60 years or older (n=340) admitted at a 630-beds tertiary hospital, located in the city of São Paulo, Brazil. A predictive model of high-risk indication was developed by analyzing logistical regression […]
Keywords: Aging; Hospital mortality; Hospitalization; lenght of stay; Logistic models; Long-term care; Patient readmission
10/Jun/2021
Impact of intensive care unit admission during handover on mortality: propensity matched cohort study
DOI: 10.31744/einstein_journal/2021AO5748
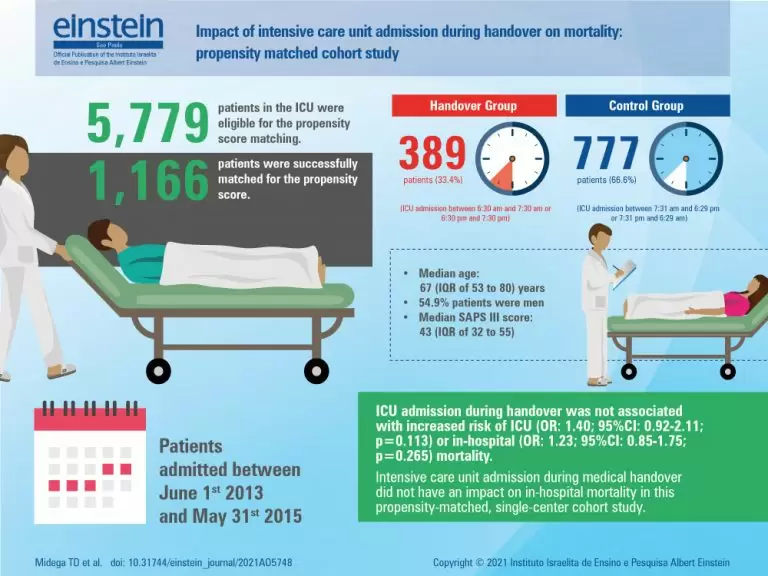
ABSTRACT Objective: To investigate the impact of intensive care unit admission during medical handover on mortality. Methods: Post-hoc analysis of data extracted from a prior study aimed at addressing the impacts of intensive care unit readmission on clinical outcomes. This retrospective, single-center, propensity-matched cohort study was conducted in a 41-bed general open-model intensive care unit. Patients were assigned to one of two cohorts according to time of intensive care unit admission: Handover Group (intensive care unit admission between 6:30 am […]
Keywords: Communication; Health resources/statistics & numerical data; Hospital mortality; Intensive care units/statistics & numerical data; Patient discharge; Patient handoff; Patient outcome assessment; Patient readmission; Patient safety
22/Jan/2013
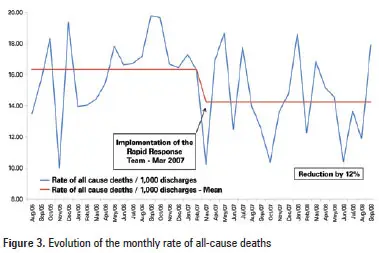
Reduced frequency of cardiopulmonary arrests by rapid response teams
DOI: 10.1590/S1679-45082012000400009
OBJECTIVE: To evaluate the impact of the implementation of a rapid response team on the rate of cardiorespiratory arrests in mortality associated with cardiorespiratory arrests and on in-hospital mortality in a high complexity general hospital. METHODS: A retrospective analysis of cardiorespiratory arrests and in-hospital mortality events before and after implementation of a rapid response team. The period analyzed covered 19 months before intervention by the team (August 2005 to February 2007) and 19 months after the intervention (March 2007 to […]
Keywords: Cardiopulmonary resuscitation; Codes; Heart arrest; Hospital mortality; Hospital rapid response team; Patient safety