einstein (São Paulo). 10/nov/2025;23:eAO1878.
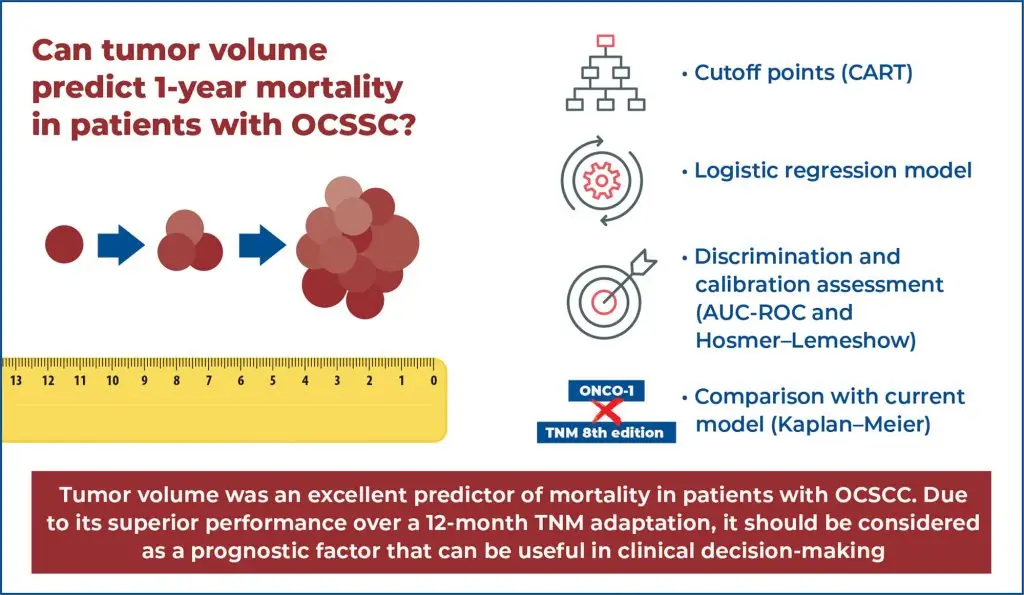
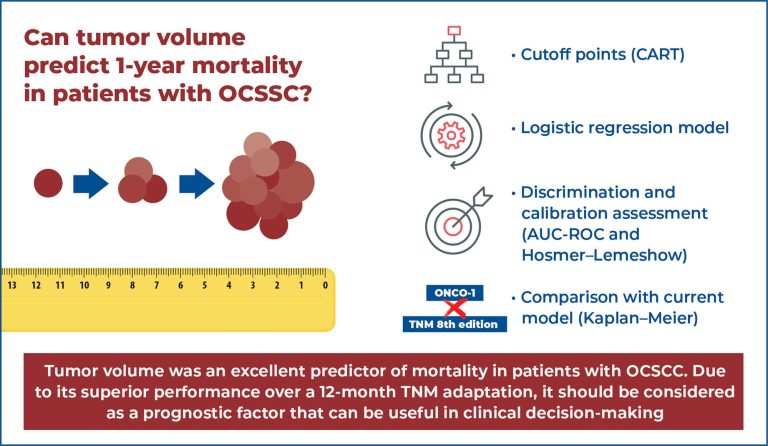
ONCO-1: Development of a univariate tool based on tumor volume to predict 1-year mortality in patients with oral cavity squamous cell carcinoma
DOI: 10.31744/einstein_journal/2025AO1878
Highlights
■ We developed ONCO-1, a simple tool based on tumor volume.
■ Cutoff points were defined by a CART model.
■ Tumor volume was a prognostic factor for 1-year mortality.
■ Tumor volume can to support clinical decision-making.
ABSTRACT
Objective:
To develop a simple and accessible univariate tool based on tumor volume to predict 1-year mortality in patients with oral cavity squamous cell carcinoma.
Methods:
A retrospective analysis was conducted on patients with oral cavity squamous cell carcinoma included in the GENCAPO cohort. Tumor volume was calculated using the formula of Monga et al. Classification and regression trees were used to define risk categories after determining the volume cutoff points. Logistic regression using 1-year vital status (alive or deceased) as the outcome was employed to construct the Oral Neoplasm Clinical Outcome in 1 year (ONCO)-1 score. Model discrimination and calibration were evaluated using the area under the receiver operating characteristic curve and the Hosmer-Lemeshow test, respectively. After building the model, we compared it with the TNM system (8th edition) using Kaplan-Meier curves.
Results:
ONCO-1 showed good stratification ability, with a progressive increase in odds ratios for 1-year mortality: odds ratio 2.47 (G2), 4.01 (G3), and 9.99 (G4), compared to group G1. The model demonstrated good discrimination (area under the curve=0.7031) and excellent calibration (Hosmer-Lemeshow p=0.99978). Kaplan-Meier curves indicated a superior prognostic performance of ONCO-1 compared to TNM classification in predicting 1-year survival.
Conclusion:
Tumor volume proved to be a robust predictor of short-term mortality in oral cavity squamous cell carcinoma. ONCO-1 provided better 1-year risk stratification compared to TNM and may contribute to more individualized clinical decision-making.
[…]
Palavras-chave: Mouth neoplasms; Carcinoma, squamous cell; Tumor burden; Prognosis; Mortality; Logistic models; Decision trees
53