einstein (São Paulo). 13/out/2025;23:eRC1216.
Difficult clinical management of groove pancreatitis: a case report
DOI: 10.31744/einstein_journal/2025RC1216
ABSTRACT
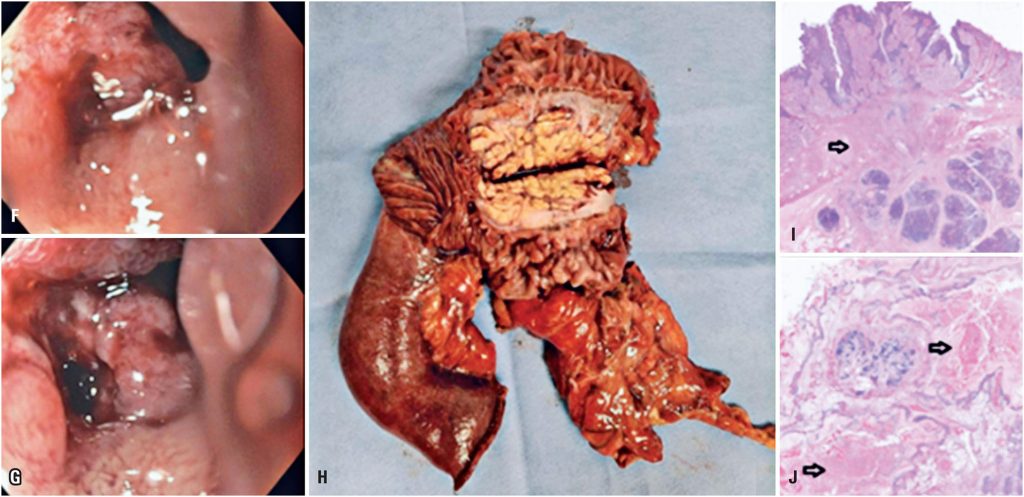
Groove pancreatitis is a rare form of chronic pancreatitis that affects the anatomical area between the head of the pancreas, medial wall of the second part of the duodenum, and common bile duct, known as the groove area. We present the case of a 40-year-old female patient with recurrent acute abdominal pain, vomiting, inappetence, and weight loss over several months. Diagnostic imaging revealed obliteration of fat in the pancreaticoduodenal groove and densification of the adjacent adipose planes, along with an infiltrative and stenosing lesion in the duodenum. Despite negative biopsy results, the patient’s symptoms persisted, leading to a multidisciplinary decision regarding surgical intervention. Initially, a less-invasive robotic gastroenteric anastomosis was performed; however, this did not yield the desired outcome. Consequently, after further episodes of pancreatic inflammation, a more extensive pancreaticoduodenectomy (Whipple procedure) was performed. The patient showed significant clinical improvement postoperatively, with no recurrence of symptoms. Groove pancreatitis poses a diagnostic challenge owing to its nonspecific clinical presentation and imaging findings. Although management typically involves dietary changes, medication, and endoscopic interventions, surgical intervention may be necessary in cases of recurrent symptoms or complications. This case highlights the importance of a multidisciplinary approach in managing groove pancreatitis and underscores the potential efficacy of surgical intervention in achieving symptomatic relief and improving quality of life, even in atypical patient demographics.
Palavras-chave: Abdominal pain; Pancreatitis, chronic
108