einstein (São Paulo). 02/fev/2026;24:eAO1720.
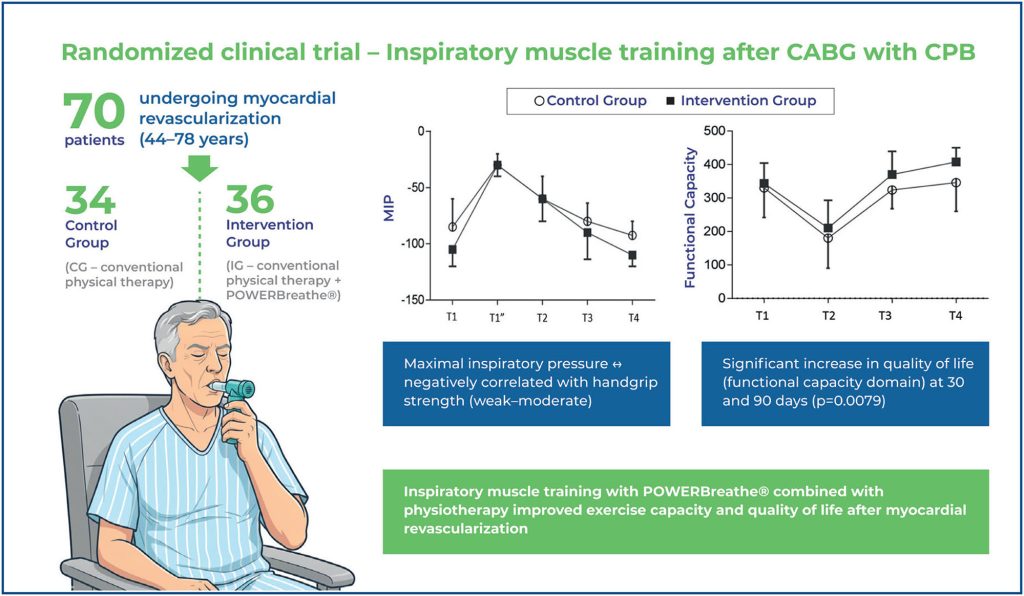
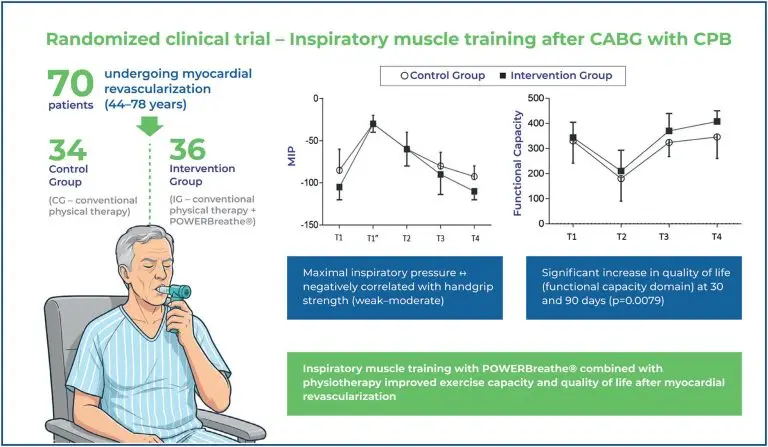
Effect of respiratory muscle training on functional capacity related to the quality of life of patients undergoing coronary artery bypass grafting with cardiopulmonary bypass: randomized clinical trial
DOI: 10.31744/einstein_journal/2026AO1720
Highlights
■ Cardiovascular diseases reduce exercise tolerance andimpair quality of life.
■ Quality of life monitoring is essential after cardiac surgery.
■ Poor postoperative quality of life predicts worse functionalrecovery.
■ Inspiratory muscle training improves exercise capacity and quality of life.
Abstract
Objective:
To evaluate the effects of inspiratory muscle training using POWERbreathe® in patients undergoing myocardial revascularization with extracorporeal circulation, focusing on respiratory and peripheral muscle strength, exercise capacity, functional independence, and quality of life, from hospitalization to a 30 and 90 day followup.
Methods:
This randomized controlled clinical trial included 70 patients aged 44-78 years who were randomized into two groups. The Control Group underwent conventional physical therapy (Control Group, n=34), whereas the Intervention Group underwent conventional physical therapy combined with inspiratory muscle training using POWERbreathe® (Intervention Group, n=36). Respiratory and peripheral muscle strength, capacity, functional independence, and quality of life were evaluated preoperatively and 5, 30, and 90 days after surgery.
Results:
A statistically significant increase in exercise capacity in the Intervention Group was observed 90 days after surgery (p=0.0192), as well as in the functional capacity domain of quality of life at 30 and 90 days after surgery (p=0.0079). The maximal inspiratory pressure and handgrip strength showed a negative correlation, ranging from weak to moderate intensity, in both groups over time.
Conclusion:
Inspiratory muscle training with the POWERBreathe combined with physical therapy improves exercise capacity and quality of life in patients undergoing myocardial revascularization.
[…]
Palavras-chave: Thoracic surgery; Breathing exercises; Rehabilitation; Physical therapy modalities
7